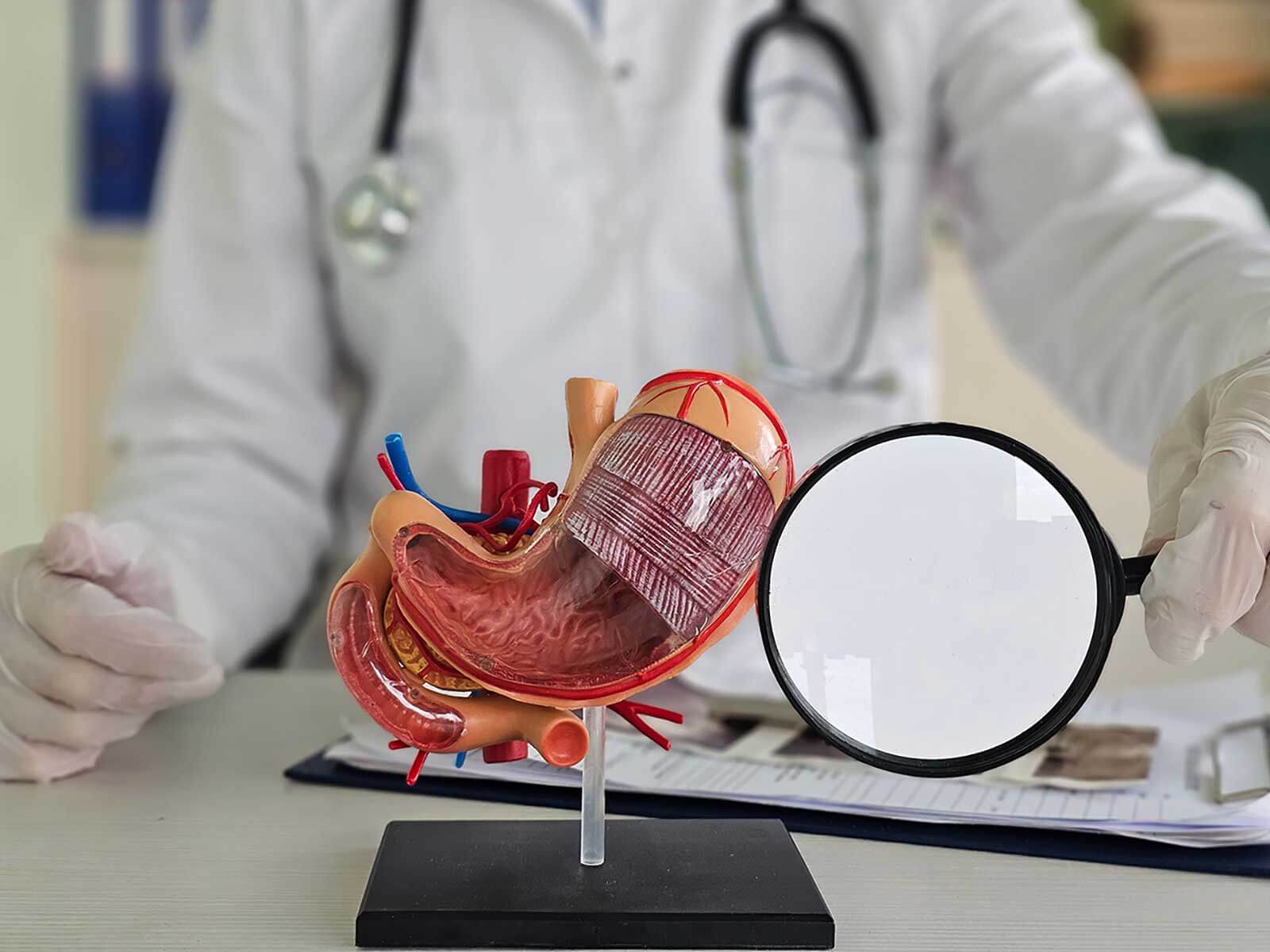
Gastric erosion without bleeding small, shallow sores on stomach lining which do not actively bleed. All these erosions are typically identified during an upper endoscopy and they are mild in nature needing attention to avoid its progression.
Symptoms may be mild to moderate and often include:
The stomach lining can be irritated resulting in erosions as a result of a variety of factors
Gastric erosion is not very uncommon and can be treated. Under proper treatment, the majority of individuals heal completely. We can help you, in case you have some symptoms, or were advised of erosions due to an endoscopy. Call GastroDoxs in Jersey Village and today make your appointment and go onto your own unique treatment plan.
We've successfully treated more than 1.5K patients, helping individuals improve their digestive health and overall well-being through expert, personalized care.
With over 20 years of experience, GastroDoxs has been a trusted provider of gastroenterology care, focusing on delivering the best outcomes for patients
Gastric erosion without bleeding are localized small and shallow mucosal lesions in the stomach which do not cause active blood loss. They are usually found during an upper endoscopy and indicate mild mucosal damage.
Bleeding ulcers penetrate deeper into the stomach wall and usually cause visible bleeding, such as blood in vomit or stool. Gastric erosions do not go deep and typically do not result in active bleeding.
Common symptoms include dull, burning pain in the upper stomach, nausea after meals, feeling full quickly, mild heartburn or indigestion, and occasional bloating.
Gastric erosion without bleeding is generally mild. However, if left untreated, it can worsen and lead to ulcers or bleeding. Most erosions heal within a few weeks with proper care.
Diagnosis is made via endoscopy, using a small camera to examine the upper stomach. Shallow sores without active bleeding are identified as gastric erosions.
Over-the-counter antacids can provide short-term relief. However, acid-lowering prescription drugs (PPIs or H2 blockers) and H. pylori antibiotics should only be taken under a physician's guidance.
Choose low-acid, soft, bland foods like oatmeal, bananas, toast, melons, pears, and lean proteins (chicken, turkey, fish). Avoid spicy, fried, tomato-based, or highly acidic foods that can irritate the stomach lining.
With proper care and lifestyle adjustments, most patients show significant improvement within two to four weeks.
Yes. A gastroenterologist can confirm the diagnosis, identify underlying factors (such as H. pylori or medication use), and develop a tailored treatment and diet plan for safe and effective healing.
Stress can increase stomach acid production, which may contribute to mucosal irritation. While stress alone does not usually cause erosions, it can exacerbate other causes like diet, medications, or infections.