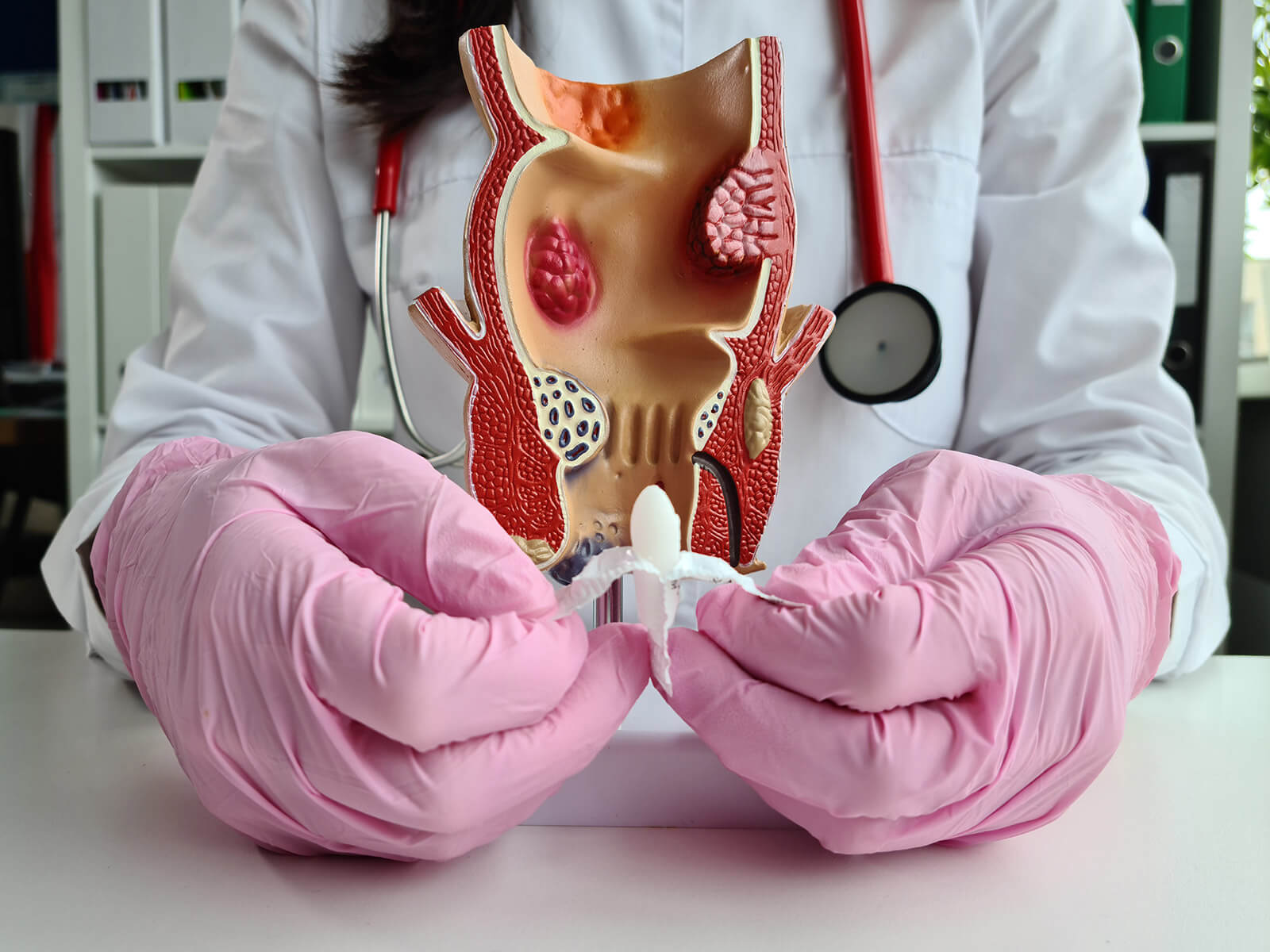
The anal fissures are small tears on the lining of the anus. They can cause a lot of pain during the passage of a bowel, passing a bowel and they can also bleed a little and pass by which makes visiting the bathroom extremely uncomfortable.
Persons with anal fissure will always complain of:
The most frequently occurring effects of anal fissures are due to:
GastroDoxs provides the combination of appropriate healthcare and study of anal fissures along with specialised treatment to Houston with attention to its patient and a good attitude on a daily basis like a tonic. We are convinced of offering caring and personal services to enable you to receive relief in the long-run and live better. Ready to stop the pain? Book an Appointment Today!
We've successfully treated more than 498 patients, helping individuals improve their digestive health and overall well-being through expert, personalized care.
With over 20 years of experience, GastroDoxs has been a trusted provider of gastroenterology care, focusing on delivering the best outcomes for patients
Simple home care measures such as stool softeners, high fiber diet, good hydration and warm sitz bath can cure acute anal fissures within 4-6 weeks.
The pain experienced on the anal fissures is normally sharp and stabbing and may have a tear which can be seen on the lining of the anus. Hemorrhoids are painful distended veins, which may come out, itch, or swell and do not necessarily give a person severe pain when discharging bowels.
An anal fissure is a tiny tear or incision in the anal lining and hemorrhoid is a blood vessels stretched out or not underneath or outside the anus. Their treatment and symptoms can have many differences.
Yes. Both hemorrhoids as well as anal fissure might exist together due to straining when a bowel movement occurs and also in case of chronic IR.
Your stool or toileting paper surface will have a bright red surface and this is a sign that it contains an anal fissure. Haemorrhoid bleeding may also be bright red in colour but it is often backed by itch, swelling or protrusion.
The late internal sphincterotomy is performed in general on persisting fissure which is not resolved despite several weeks of topical interventions (nitrates, calcium channel blockers), sitz baths, or Botox injections.
Bulk-forming laxatives (e.g., polyethylene glycol) should be recommended as bulk forming agents that may help to produce soft and easy-to-pass stools and relieve pressures in the fissure.
Your gastroenterologist may begin with the topical nitroglycerin ointment or calcium blocking agent such as diltiazem to dilation of anal sphincter and cause healing.
A small incision into the internally anal sphincter muscle would be termed as lateral internal sphincterotomy to reduce the resting pressure and improve the blood supply to the area and heal the fissure.
A few of these prevention strategies include eating food that is high in fiber content, a high level of hydration, not straining during bowel movements, use of Stool softeners where necessary and taking warm sitz baths after attending to the bowel movements.