What Is Pelvic Pain?
Pelvic pain is discomfort in the lower belly, between the hips. It may be sharp, dull, steady, or come and go. Both men and women in Houston can experience pelvic pain. The ICD-10 code R10.2 is used for pelvic and perineal pain. If the pain persists for more than six months, it's classified as chronic pelvic pain syndrome.
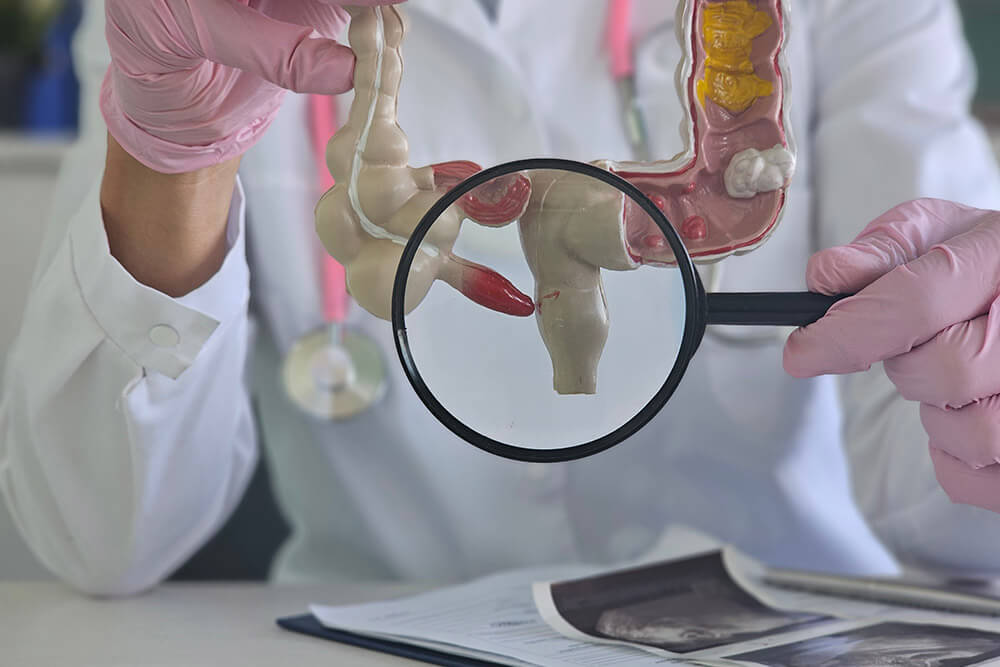
Common Causes and Risk Factors
- Gynecologic conditions - Like endometriosis or pelvic inflammatory disease (PID)
- Urologic issues - Such as chronic prostatitis or bladder pain
- Digestive problems - Including irritable bowel syndrome (IBS)
- Muscle strain - From tight or weak pelvic floor muscles
- Other risks - Past surgeries, infections, or high stress levels
Signs and Symptoms
- Ongoing dull ache or sharp pain in the lower belly
- Pain during or after sex
- Burning or urgency when urinating
- Bloating, gas, or a sensation of pressure
- Pain during bowel movements
How Dr. Rishi Chadha Diagnoses Pelvic Pain?
Dr. Chadha uses a step-by-step approach:
Symptom Review & Medical History
He begins by discussing your pain pattern, duration, intensity, and any past surgeries or infections.
Physical Examination
A focused exam evaluates pelvic tenderness, muscle tightness, and floor-muscle function.
Laboratory Tests
- Blood tests to check for infection or inflammation.
- Urinalysis to rule out urinary tract infection or prostatitis.
Imaging Studies
- Pelvic ultrasound or MRI to identify endometriosis, masses, or other structural issues.
Endoscopic Evaluation (if needed)
Colonoscopy or upper endoscopy to investigate digestive-related pain sources.
Pelvic Floor Assessment
Referral for specialized pelvic floor therapy to assess tight or weak muscles.
Frequently Asked Questions
What is chronic pelvic pain syndrome?
It's pain in the pelvic area lasting more than six months, even after treatment.
Can pelvic pain after sex be treated?
Yes. Diet, physical therapy, and medication often help ease this pain.
How is chronic prostatitis diagnosed?
With your symptoms, a physical exam, urine tests, and sometimes a prostate massage.
Is an ICD-10 code required for insurance?
Yes. R10.2 helps with insurance approval for tests and treatments.
Will I need surgery?
Most patients improve without it. Diet and non-surgical options usually work well.
How long before I feel better?
Many patients feel better within 4 to 12 weeks, depending on the cause.
Are diet changes really helpful?
Yes. A low-FODMAP diet often reduces IBS-related pain.
Do you offer pelvic floor therapy?
Yes. We work with local experts for therapy that strengthens or relaxes pelvic muscles.
Will the pain come back?
With the right plan and follow-up, many patients stay pain-free long term.
How should I prepare for my visit?
Bring a list of symptoms, past test results, and a few days of your food diary.