Diverticulitis is a scary condition. You can ask yourself: Is diverticulitis a self-limiting condition? We would be happy to answer you (at Gastrodoxs) in a straightforward, friendly way. In this article, we are going to take a stroll through the definition of what is diverticulitis and the difference between it and diverticulosis as well as some tips on how you can relieve it. You are also going to read quotes of Dr. Bharat Pothuri, a reputable Houston gastroenterologist, about his opinions.
Regardless of whether you are living in Montrose, Sugar land or the Woodlands, this guide is made to suit the needs of people within Houston who are interested in a straightforward piece of advice that is not theoretical. Let's dive in.
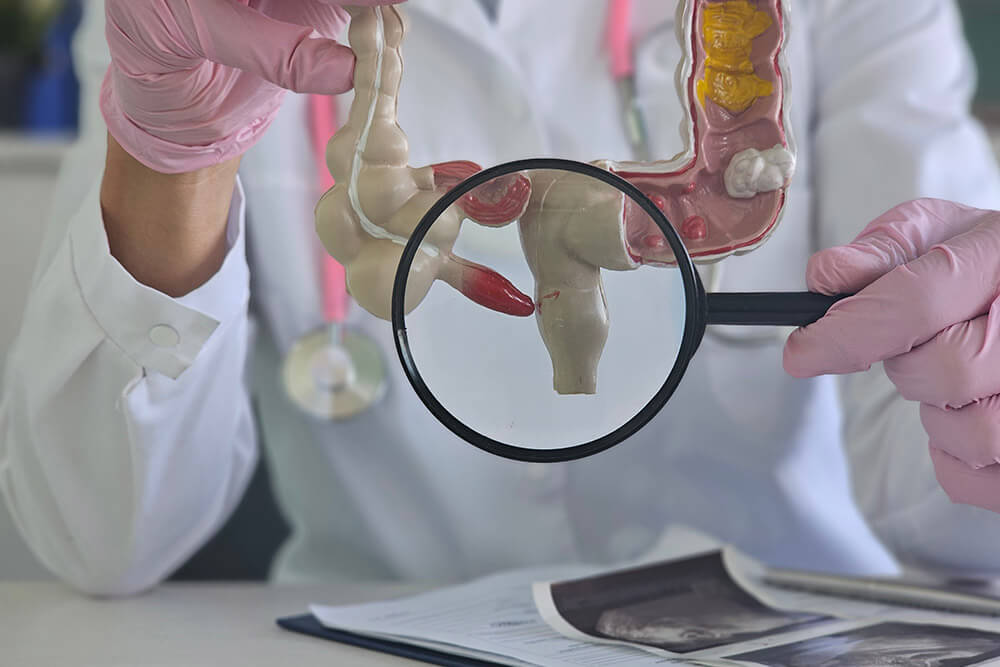
It all starts in your colon. They might be tiny cysts located in the lining of your digestive tract known as the diverticula. The absence of problems leads to the term diverticulosis. Should those pouches inflame or be infected, then that is diverticulitis .
| Characteristics | Diverticulosis | Diverticulitis |
| Definition | Pouches (diverticua) presence | Inflammation or infection of pouches |
| Symptoms | Usually none | Lower abdominal pain, fever, nausea |
| Possibility of Complications | Low | Higher-abscess, perforation |
| Treatment | Dietary High-fiber, changes in lifestyle | Antibiotics, clear liquids, may include surgery |
| Prevalence in Houston | Common in adults older than 40 years of age | Affects approximately 1025% of the diverticulosis population |
Diverticulosis as explained by Dr. Bharat Pothuri is a silent disease. You do not even know that it is usually there until the onset of diverticulitis.
The major question: is diverticulitis self-limiting? In minor cases, other individuals experience relief through home care. However, you are never supposed to disregard symptoms.
Dr. Pothuri is an expert in gastroenterology based in Houston, he rarely recommends self-treatment. You are supposed to keep in touch with your provider even when the symptoms are alleviated.
Most of the symptoms are conspicuous; others are latent. Back pain is one of those that makes one surprised.
Back pain may develop when inflammation agitates in the area of nerves. In case of an unexplained lower back pain, accompanied by abdominal pain, then diverticulitis should be on your watchlist.
The other common question is how long do diverticulitis last? The solution depends on the severity and treatment.
Typical timelines:
According to Dr. Pothuri, recovery is less when it is undertaken early. When patients adhere to dietary recommendations and take all medications, most of them begin to feel better after approximately one week.
It is important to know triggers so that you will avoid attack in the future. The reasons to exacerbation of diverticulitis include some of the following:
According to Dr. Pothuri, lifestyle is important. It is tempting to avoid healthy options in the hectic life of Houston, but this can be a welcoming invitation to a flare-up
In case you happen to reside in Houston, then you are lucky to be in the locality of the best medical facilities such as Houston Methodist, Memorial Hermann and the Texas Childrens Hospital (in cases involving children). This is how treatment usually spells like:
The best thing is to prevent than to cure. These tips are long-term gut health tips to embrace:
The humid dissipation of the summer in Houston and its busy life may influence your routine. Here's how to adapt:
Although diverticulitis can even go away, do not put off seeking help in such cases:
In case you have these red flags, go to the closest area of Houston which happens to be the Memorial Hermann or the Lyndon B. Johnson Hospital that operates 24/7.
In a brief conclusion, we would like to review in simple words the difference between diverticulitis and diverticulosis:
Diverticulitis does not necessarily resolve itself. Through appropriate treatment, diet and lifestyle modification, you can cure and minimize the risk of a flare-up. In case you are in Houston, get the local specialists, such as Dr. Bharat Pothuri, and the best healthcare facilities. Keep updated, keep active and keep in mind that Gastrodoxs is there to help you on your digestive health walk.
Light cases of diverticulitis can be alleviated by rest and clear liquid diet, and you must never ignore a physician.
Pouches in the colon are called diverticulosa; inflammation or infection of the pouches are known as diverticulitis.
Yes. Inflammation may also cause irritation of the surrounding nerves causing lower back pain.
Symptoms could last weeks without treatment and be life threatening.
Majority of the people get better within 7-10 days under administration of prescribed antibiotics and dietary instructions.
This can be caused by low fiber, constipation, some medications, obesity, smoking, stress and insomnia.
Recent studies indicate that nuts and seeds do not trigger the attacks. Nevertheless, adhere to the eating plan of your physician.
Probiotics, high-fiber diets, and fluid replacement can work, but they do not substitute medical assistance.
Emergency treatment is needed in case of severe pain, high fever, vomiting, or bloody diarrhea.
Visit Gastrodoxs to get referrals or to ask your physician in primary care to refer you to a gastroenterologist.