What Is Pancreatitis?
Pancreatitis is swelling or irritation of the pancreas. The pancreas is a small organ behind your stomach. It helps you digest food and control blood sugar with insulin. When inflamed, it can cause pain and serious health issues. Some cases are mild. Others may be severe or life-threatening.
Common Causes and Risk Factors
- Gallstones - Can block flow and trigger an attack
- Heavy alcohol use - Often leads to chronic pancreatitis
- High triglycerides - Levels above 1,000 mg/dL raise risk
- Some medications - Certain drugs may harm the pancreas
- Genetic mutations - Rare genes may raise your chance
- Smoking - Makes inflammation worse and harder to treat
Signs and Symptoms
- Upper belly pain that may reach your back
- Nausea and vomiting
- Fever or fast heartbeat
- A bloated or tender stomach
- Ongoing weight loss in chronic cases
How Dr. Rishi Chadha Diagnoses Pancreatitis?
Dr. Chadha uses a step-by-step approach:
Medical History and Examination
He reviews your symptoms, dietary habits, alcohol use, family history and other risk factors that could trigger pancreatitis.
Blood Tests
Checks pancreatic enzyme levels (amylase and lipase) and triglycerides to confirm inflammation and rule out other causes.
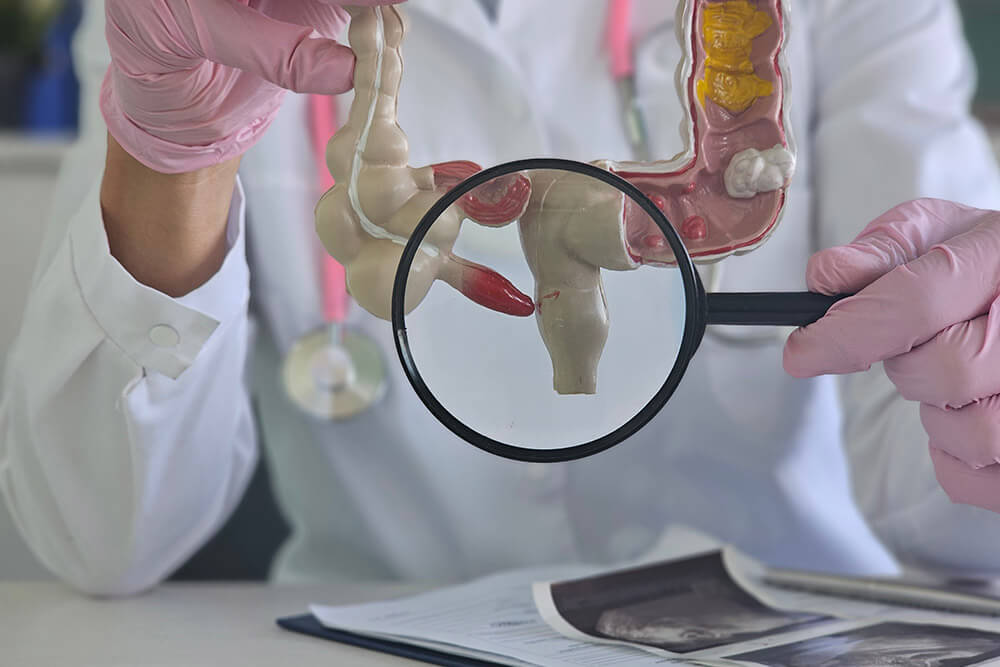
Imaging Studies
- Abdominal ultrasound to detect gallstones and swelling of the pancreas.
- CT scan for detailed imagery-identifying fluid collections, necrosis, or complications.
Endoscopic Ultrasound (EUS) and ERCP
Uses EUS for a close-up view of the pancreas and ducts. ERCP is performed if there's a ductal blockage-allowing stone removal or stent placement.
Frequently Asked Questions
Can pancreatitis be deadly?
Yes, serious cases can be life-threatening. Prompt diagnosis and treatment help lower that risk.
What is the ICD-10 code for acute pancreatitis?
The codes range from K85.0 to K85.9, depending on the underlying cause of the acute attack.
What is the ICD-10 code for chronic pancreatitis?
Chronic pancreatitis is classified under K86.1 in the ICD-10 system.
What are the four stages of acute pancreatitis?
The progression includes mild swelling, tissue necrosis (death), infection, and potential long-term complications.
Can pancreatitis be cured?
There's no definitive cure, but symptoms and complications can be effectively managed with lifestyle changes, medications, and procedures.
How long does recovery take?
Mild cases often improve within about one week. Severe or complicated cases may require several weeks to months of care.
Is pancreatitis genetic?
Yes. Rare gene mutations can increase your risk of developing pancreatitis, particularly chronic forms.
Can I drink alcohol again?
No. Complete abstinence from alcohol is crucial to prevent future attacks and protect pancreatic health.
When is ERCP needed?
Dr. Chadha may recommend ERCP if imaging shows a duct blockage or gallstones that need to be removed or duct flow improved.
Will I need surgery?
Surgery is reserved for cases that don-t respond to medical or endoscopic treatments, or when complications like persistent blockages arise.