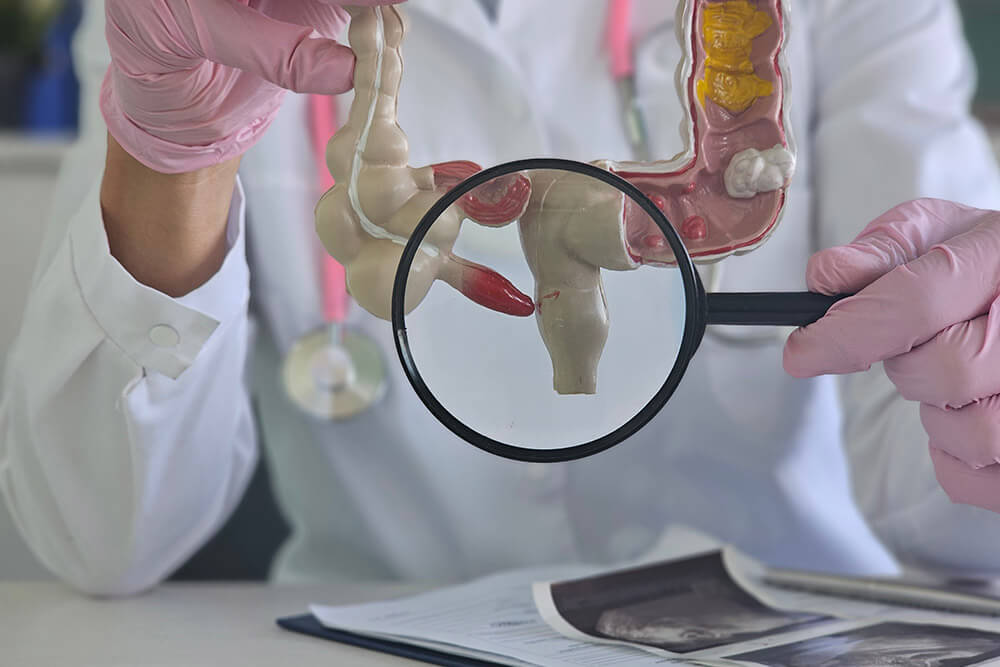
What Is an Ileal Stricture?
An ileal stricture is a narrowing in the last part of your small intestine, called the ileum. This tight segment can block or slow the passage of food, leading over time to symptoms such as pain, bloating and other digestion problems.
Common Symptoms
- Pain or cramps in the lower right abdomen
- Bloating, especially after meals
- Feeling full quickly when eating
- Nausea or vomiting
- Diarrhea or constipation
- Unplanned weight loss
What Causes Ileal Strictures?
- Crohn's disease - Chronic inflammation leads to scar tissue formation and narrowing of the bowel. (ICD-10: K50.019)
- Past surgeries, infections or radiation - Damage to the intestinal wall can result in fibrotic strictures.
- Family history - A relative with inflammatory bowel disease (IBD) raises your risk.
- Smoking and NSAID use - Both can irritate your gut lining and worsen inflammation.
How Dr. Rishi Diagnoses Ileal Stricture?
Health History & Physical Exam
Dr. Chadha begins by reviewing your symptoms, Crohn's or IBD history, prior surgeries or infections, family risk factors, lifestyle habits, and a focused abdominal exam to pinpoint discomfort or signs of obstruction.
Blood Tests
Lab work checks for elevated inflammatory markers (CRP, ESR), anemia from chronic blood loss, and nutritional deficiencies that often accompany strictures.
Imaging Tests
- CT Scan - Visualizes narrowed segments, inflammation, and any upstream dilation.
- MR Enterography - Offers high-resolution images of the small bowel without radiation, highlighting strictures and active disease.
Endoscopy or Colonoscopy
A flexible scope is passed through the mouth (upper endoscopy) or rectum (colonoscopy) to directly view and measure the ileal narrowing, assess its length, and take biopsies if needed.
ICD-10 Documentation
Precise coding (e.g., K50.019 for Crohn's with ileal stricture) ensures accurate records for treatment planning and insurance authorization.

Frequently Asked Questions
What is an ileal stricture?
It's a narrowing in the last part of the small intestine (the ileum) that can block or slow the passage of food.
What causes an ileal stricture?
Chronic inflammation from Crohn's disease is the most common cause. Past surgeries, infections, radiation, family history of IBD, smoking, and NSAID use can also lead to strictures.
What are the symptoms?
Common signs include lower right abdominal pain or cramps, bloating after meals, early satiety, nausea or vomiting, diarrhea or constipation, and unintentional weight loss.
How is an ileal stricture diagnosed?
Diagnosis involves a detailed health history and exam, blood tests for inflammation or anemia, imaging (CT scan or MR enterography), and endoscopy or colonoscopy to visualize and measure the narrowing.
When is surgery needed?
Surgery is considered if medications and endoscopic dilation don-t relieve symptoms or clear the blockage. Options include strictureplasty, laparoscopic resection, or open surgery.
Can diet help with symptoms?
Yes. Eating small, soft, low-fiber meals, staying hydrated, and avoiding gas-forming or fizzy drinks can ease discomfort during flare-ups.
What is the ICD-10 code for an ileal stricture due to Crohn's disease?
The ICD-10 code for Crohn's disease with an ileal stricture is K50.019.
How long does recovery take after endoscopic dilation?
Most patients return to normal activities within 1 to 3 days after dilation.
Is endoscopic dilation safe?
Yes. It's a minimally invasive procedure with a low risk of complications. Rarely, bleeding or a small tear (perforation) may occur.
Will insurance cover tests and treatments?
Most insurance plans cover diagnostic tests and treatments for ileal strictures. Our team will assist you in verifying your coverage.