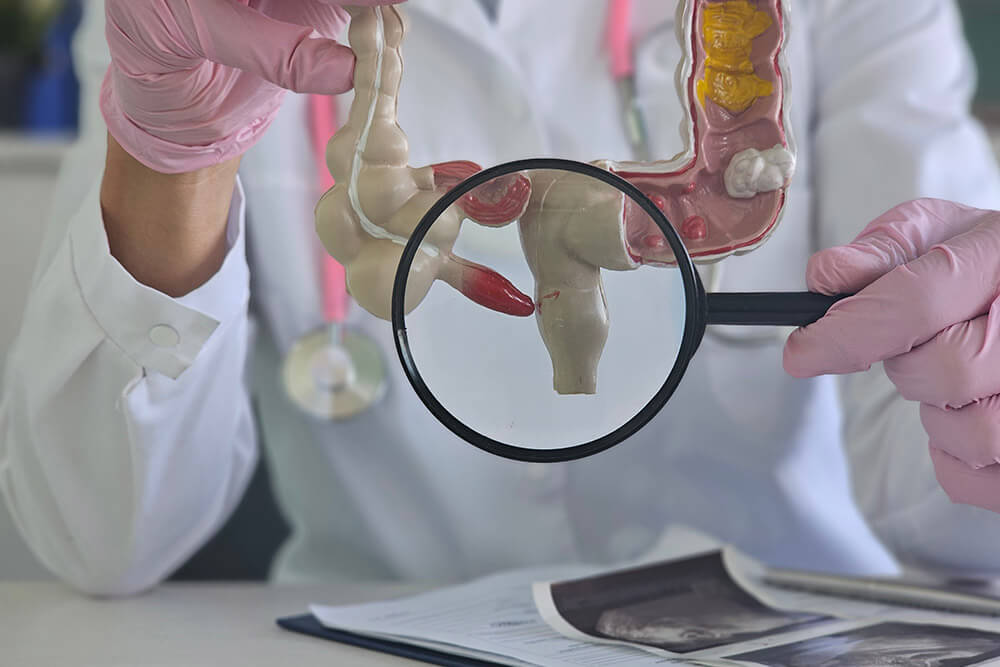
What Is Diverticulitis?
Diverticulitis happens when small pouches (diverticula) in the colon wall become inflamed or infected. During an attack, you may experience belly pain, fever, and changes in bowel habits. With prompt treatment, most people recover quickly.
Common Causes and Risk Factors
- Age : More common after 40
- Low-fiber diet : Hard stools raise colon pressure
- Obesity or smoking : Increases your risk
- Family history : Genetics can play a part
- Chronic constipation : Straining can worsen pouches
Signs and Symptoms
- Sharp pain in the lower left abdomen
- Fever, chills, or malaise
- Bloating, gas, or abdominal cramps
- Diarrhea or constipation
- Thin, lumpy stool or mucus in the stool
How Dr. Rishi Diagnoses Diverticulitis?
Step-by-Step Approach:
Medical History & Physical Exam
Dr. Chadha reviews your symptoms (pain location, fever, bowel changes), diet, lifestyle and performs a gentle abdominal exam to pinpoint tenderness or guarding.
Blood Tests
Complete blood count (CBC) and inflammatory markers (CRP) help detect infection or inflammation.
Imaging Studies
- CT Scan : The gold standard to visualize diverticula, wall thickening, abscesses or complications.
- Ultrasound : May be used in selected cases to identify localized inflammation or fluid collections.
Endoscopic Evaluation
Once acute inflammation has subsided, a colonoscopy is performed to rule out other causes (polyps, cancer) and assess overall colon health.
Frequently Asked Questions
What is diverticulitis?
Diverticulitis is the infection or inflammation of small pouches (diverticula) that form in the colon wall.
What causes it?
Low-fiber diets, aging (over 40), obesity, smoking, family history, and chronic constipation can increase your risk.
What does it feel like?
Sharp pain in the lower left abdomen, fever, chills, bloating, gas, and sometimes changes in bowel habits.
Can it go away?
Yes. Most cases improve with rest, antibiotics, and dietary changes, though some people may have recurrent episodes.
How can I ease pain fast?
Drink clear fluids, rest, apply a heating pad to your abdomen, and use acetaminophen for pain relief.
What does my stool look like?
It may be thin, lumpy, or contain mucus during a flare-up.
What is the ICD-10 code?
K57.20 is used for diverticulitis without perforation or abscess on medical records.
Should I change my diet?
Yes. Start with clear liquids during a flare, then gradually add high-fiber foods like fruits, vegetables, beans, and whole grains.
When should I see a doctor?
If you experience high fever, severe abdominal pain, persistent nausea/vomiting, or significant changes in bowel habits.
Can surgery fix it?
For recurrent or complicated cases, surgical removal of the affected colon segment can prevent future flare-ups.