How Dr. Nghia Nguyen Diagnoses Intestinal Lymphangiectasia?
Dr. Nguyen uses a step-by-step approach:
Medical History and Physical Exam
He reviews your symptoms (diarrhea, swelling, fatigue), growth history, family history, and any prior heart, infection, or cancer issues. He performs a targeted abdominal exam to check for edema and malnutrition.
Blood Tests
We measure serum albumin, total protein, lymphocyte count, and fat-soluble vitamin levels (A, D, E, K) to assess protein loss and malabsorption.
Stool Fat Analysis
A 72-hour stool collection quantifies fecal fat, confirming fat malabsorption.
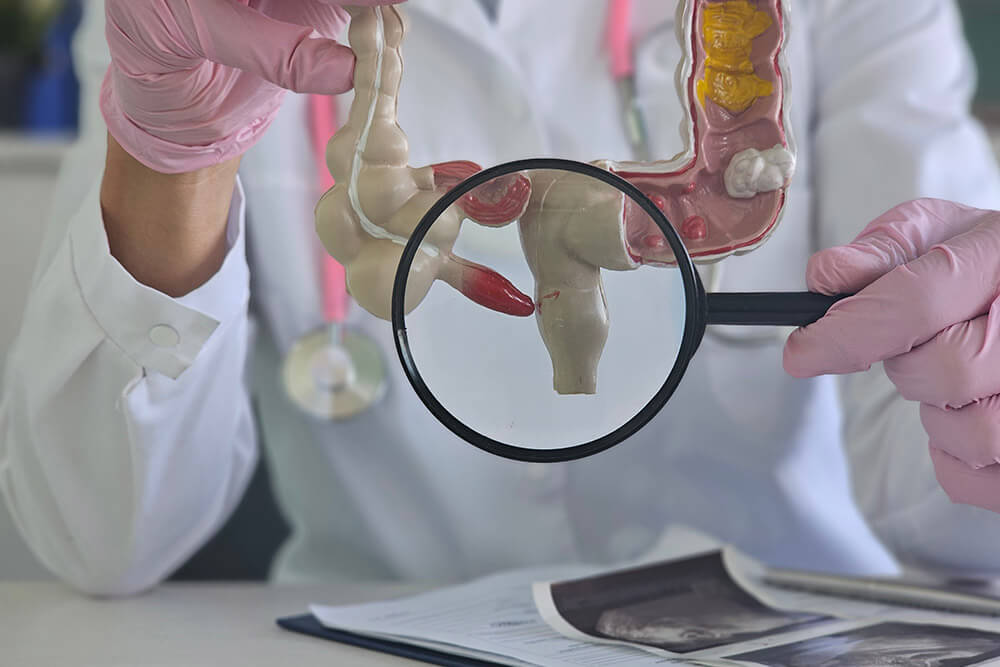
Endoscopy and Biopsy
An upper GI endoscopy allows direct visualization of the small intestinal mucosa. Duodenal biopsies are taken to look for dilated lymphatic channels (lacteal dilation).
Imaging Studies
- MR lymphangiography or CT enterography to map lymphatic vessels and detect leaks or blockages.
- Fluoroscopic lymphangiogram or ultrasound‐guided lymphatic embolization planning when intervention is needed.
Advanced Testing (if needed)
In rare cases, lymphoscintigraphy or direct lymphatic cannulation is used to pinpoint leak sites before embolization.

How Dr. Nghia Nguyen Diagnoses?
Dr. Nguyen uses a systematic approach:
Medical History and Physical Exam
He characterizes the pain (onset, location, duration, triggers), reviews medications, alcohol use, NSAID exposure, and checks for tenderness or guarding in the epigastric region.
Laboratory Tests
- Complete blood count (CBC) to assess for anemia or infection
- Liver function tests (LFTs), amylase, lipase to screen for hepatobiliary or pancreatic causes
- H. pylori stool antigen or breath test if ulcer disease is suspected
Imaging Studies
- Abdominal ultrasound to look for gallstones, biliary sludge, or liver abnormalities
- CT scan of the abdomen/pelvis if pancreatitis, mass, or other intra-abdominal pathology is suspected
Upper Endoscopy (EGD)
Direct visualization of the esophagus, stomach, and duodenum to identify peptic ulcers, gastritis, esophagitis, or tumors. Biopsies can be obtained for H. pylori and histology.
Advanced Testing (if needed)
Ambulatory pH monitoring or high-resolution manometry for reflux or motility disorders; HIDA scan for gallbladder function; or referral for surgical evaluation if structural disease is found.

Frequently Asked Questions
What causes intestinal lymphangiectasia?
It can be primary (present at birth due to malformed lymph vessels) or secondary (from heart disease, infections, tumors, radiation, or surgery that damage the lymphatic system).
How is intestinal lymphangiectasia diagnosed?
Diagnosis involves blood tests for protein and vitamin levels, stool fat analysis, endoscopy with biopsy, and imaging studies (MRI or CT) to locate lymph leaks or blockages.
What diet should patients follow?
A low-fat, high-protein diet is key. Avoid long-chain fats and use MCT oil instead. Recommended foods include egg whites, skinless chicken, white rice, cooked vegetables, and non-fat dairy. Supplementation with vitamins A, D, E, and K is often needed.
What medications are used in treatment?
Dr. Nguyen may prescribe diuretics to reduce swelling, octreotide to slow lymph flow, IV albumin for very low protein levels, and daily vitamin/mineral supplements to prevent deficiencies.
When are advanced treatments like embolization or surgery needed?
If diet and medications fail to control symptoms, lymphatic embolization can seal leaking vessels. In rare cases of severe intestinal damage, surgical resection may be considered.
Can I live a normal life with this condition?
Yes. With early diagnosis, dietary management, and appropriate therapies, most patients lead healthy, active lives and maintain good nutrition.