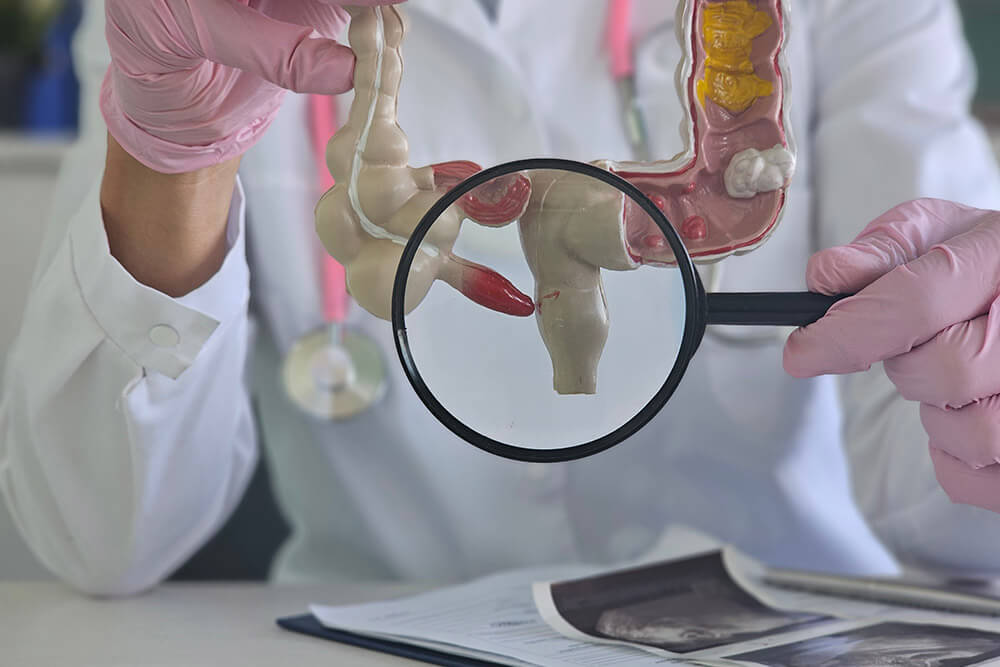
What Is Diverticulitis?
Diverticulitis develops when small pouches (diverticula) along the colon wall become inflamed or infected, leading to abdominal pain and digestive upset.
Common Causes and Risk Factors
- Age-related weakening of the colon wall (more common over 40)
- Low-fiber diet that leads to harder stools and increased colon pressure
- Physical inactivity or a sedentary lifestyle
- Obesity or being overweight
- Smoking tobacco
- Certain medications (e.g., steroids, NSAIDs)
Signs and Symptoms
- Sharp or steady pain in the lower left abdomen
- Fever and chills
- Nausea or vomiting
- Constipation or diarrhea
- Abdominal tenderness when pressed
Expert Treatment for Diverticulitis by Dr. Bharat Pothuri
Step 1: Medical History and Physical Exam
Dr. Pothuri starts by asking questions about your health and symptoms. He will gently press on your belly to check for pain.
Step 2: Imaging
To confirm the diagnosis, he may order a CT scan. This shows swelling and any infection. In some cases, an ultrasound is helpful.
Step 3: Blood Tests
He might also order blood tests to look for signs of illness.
Step 4: Follow-up Evaluation
After you feel better, a colonoscopy may be done to check for other problems.
Frequently Asked Questions
What causes a diverticulitis flare-up?
Low fiber intake, dehydration, lack of exercise, or sudden diet changes can increase pressure in the colon and trigger inflammation.
How is diverticulitis treated?
Mild cases often respond to antibiotics and rest. More severe cases may need fluid drainage or surgery to repair complications.
Can diverticulitis cause strong stomach pain?
Yes. The pain is typically sharp and steady on the lower left side of the abdomen and can be intense during an attack.
When should I go to the hospital?
If you experience high fever, severe abdominal pain, persistent vomiting, or signs of bleeding, seek immediate medical care.
What should I eat during recovery?
Begin with clear liquids, then progress to low-fiber foods. Gradually reintroduce fruits, vegetables, and whole grains as your symptoms improve.
How can I prevent future flare-ups?
Maintain a high-fiber diet, stay well hydrated, exercise regularly, and manage stress to support healthy colon function.
Do I need a colonoscopy after a diverticulitis episode?
Yes. A colonoscopy is recommended once you've healed to check for polyps, cancer, or other underlying issues.